Definition
Diabetes mellitus type 2 is a chronic condition that affects the way your body metabolizes sugar (glucose), your body”s main source of fuel.
With diabetes mellitus type 2, your body either resists the effects of insulin or doesn”t produce enough insulin to maintain a normal glucose level. Untreated, diabetes mellitus type 2 can be life-threatening.
There”s no cure for diabetes mellitus type 2, but you can manage or even prevent the condition. Start by eating well, exercising and maintaining a healthy weight. If diet and exercise aren”t enough to control your diabetes mellitus type 2, you may need diabetes medications or insulin therapy to manage your blood sugar.
Symptoms
Diabetes mellitus type 2 symptoms may develop very slowly. In fact, you can have diabetes mellitus type 2 for years and not even know it. Look for:
- Increased thirst and frequent urination.
- Increased hunger.
- Weight loss.
- Fatigue.
- Blurred vision.
- Slow-healing sores or frequent infections.
- Areas of darkened skin.
Causes
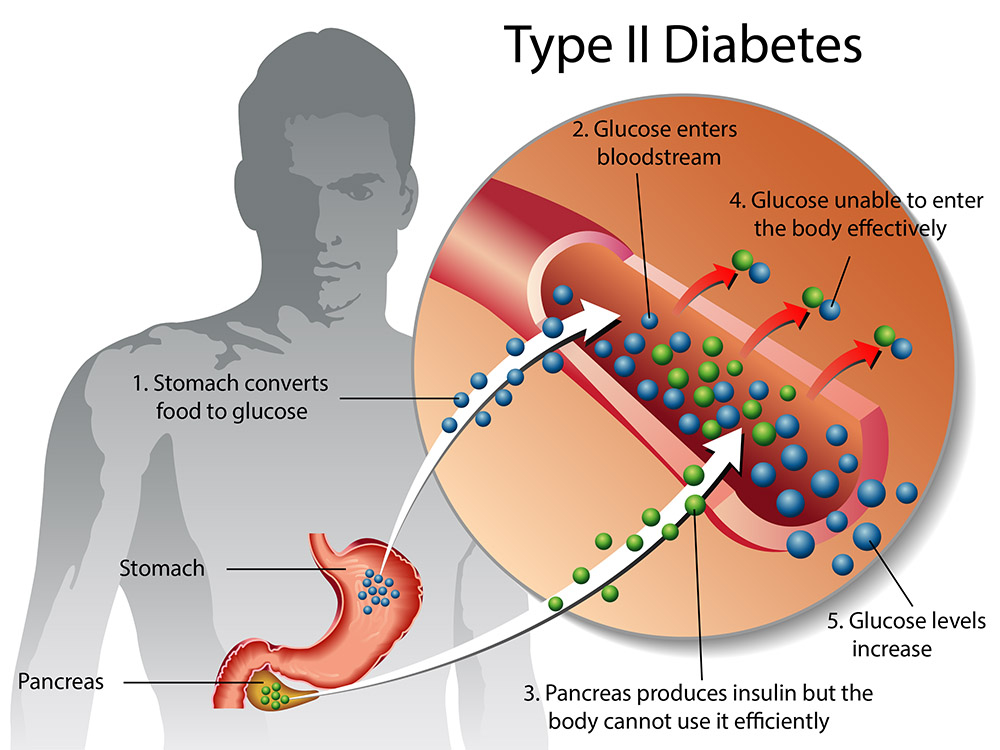
- Diabetes mellitus type 2 develops when the body becomes resistant to insulin or when the pancreas stops producing enough insulin. Exactly why this happens is unknown, although excess weight and inactivity seem to be contributing factors.
- Insulin is a hormone that comes from the pancreas, a gland situated just behind and below the stomach. When you eat, the pancreas secretes insulin into the bloodstream. As insulin circulates, it acts like a key by unlocking microscopic doors that allow sugar to enter your cells. Insulin lowers the amount of sugar in your bloodstream. As your blood sugar level drops, so does the secretion of insulin from your pancreas.
- Glucose is a main source of energy for the cells that make up muscles and other tissues. Glucose comes from two major sources: the food you eat and your liver. After intestinal digestion and absorption, sugar is absorbed into the bloodstream. Normally, sugar then enters cells with the help of insulin.
- The liver acts as a glucose storage and manufacturing center. When your insulin levels are low the liver metabolizes stored glycogen into glucose to keep your glucose level within a normal range.
- In diabetes mellitus type 2, this process works improperly. Instead of moving into your cells, sugar builds up in your bloodstream. This occurs when your pancreas doesn”t make enough insulin or your cells become resistant to the action of insulin.
- In type 1 diabetes, which is much less common, the pancreas produces little or no insulin.
Risk factors
Researchers don”t fully understand why some people develop diabetes mellitus type 2 and others don”t. It”s clear that certain factors increase the risk, however, including:
- Weight: Being overweight is a primary risk factor for diabetes mellitus type 2. The more fatty tissue you have, the more resistant your cells become to insulin.
- Fat distribution: If your body stores fat primarily in your abdomen, your risk of diabetes mellitus type 2 is greater than if your body stores fat elsewhere, such as your hips and thighs.
- Inactivity: The less active you are, the greater your risk of diabetes mellitus type 2. Physical activity helps you control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
Family history: The risk of diabetes mellitus type 2 increases if your parent or sibling has diabetes mellitus type 2. - Race: Although it”s unclear why, people of certain races — including blacks, Hispanics, American Indians and Asian-Americans — are more likely to develop diabetes mellitus type 2 than whites are.
- Age: The risk of diabetes mellitus type 2 increases as you get older, especially after age 45. That”s probably because people tend to exercise less, lose muscle mass and gain weight as they age. But diabetes mellitus type 2 is also increasing dramatically among children, adolescents and younger adults.
- Prediabetes: Prediabetes is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes mellitus type 2. Left untreated, prediabetes often progresses to diabetes mellitus type 2..
Complications
Diabetes mellitus type 2 can be easy to ignore, especially in the early stages when you”re feeling fine. But diabetes affects many major organs, including your heart, blood vessels, nerves, eyes and kidneys. Controlling your blood sugar levels can help prevent these complications.
Although long-term complications of diabetes develop gradually, they can eventually be disabling or even life-threatening. Some of the potential complications of diabetes include:
- Heart and blood vessel disease: Diabetes dramatically increases the risk of various cardiovascular problems, including coronary artery disease with chest pain, heart attack, stroke, narrowing of arteries (atherosclerosis) and high blood pressure.
- Nerve damage: Excess sugar can injure the walls of the tiny blood vessels (capillaries) that nourish your nerves, especially in the legs. This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward. Poorly controlled blood sugar can eventually cause you to lose all sense of feeling in the affected limbs. For men, erectile dysfunction may be an issue.
- Kidney damage: The kidneys contain millions of tiny blood vessel clusters that filter waste from your blood. Diabetes can damage this delicate filtering system. Severe damage can lead to kidney failure or irreversible end-stage kidney disease, requiring dialysis or a kidney transplant.
- Eye damage: Diabetes can damage the blood vessels of the retina, potentially leading to blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
Foot damage: Nerve damage in the feet or poor blood flow to the feet increases the risk of various foot complications. Left untreated, cuts and blisters can become serious infections. Severe damage might require toe, foot or even leg amputation. - Skin and mouth conditions: Diabetes may leave you more susceptible to skin problems, including bacterial and fungal infections. Gum infections also may be a concern, especially if you have a history of poor dental hygiene.
- Osteoporosis: Diabetes may lead to lower than normal bone mineral density, increasing your risk of osteoporosis.
Alzheimer”s disease: Diabetes mellitus type 2 may increase the risk of Alzheimer”s disease and vascular dementia. Cardiovascular problems caused by diabetes could contribute to dementia by blocking blood flow to the brain or causing strokes. - Hearing problems: Diabetes can also lead to hearing impairment.
Tests and Diagnosis
For Diabetes mellitus type 2, the recommended testing includes:
- Glycated hemoglobin (A1C) test: This blood test indicates your average blood sugar level for the past two to three months. It works by measuring the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells. The higher your blood sugar levels, the more hemoglobin you”ll have with sugar attached. An A1C level of 6.5 percent or higher on two separate tests indicates you have diabetes. A result between 5.7 and 6.4 percent is considered prediabetes, which indicates a high risk of developing diabetes. Normal levels are below 5.7 percent.
- Random blood sugar test: A blood sample will be taken at a random time. Blood sugar values are expressed in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). Regardless of when you last ate, a random blood sugar level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes, especially when coupled with any of the signs and symptoms of diabetes, such as frequent urination and extreme thirst. A level between 140 mg/dL (7.8 mmol/L) and 199 mg/dL (11.0 mmol/L) is considered prediabetes, which puts you at greater risk of developing diabetes. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal.
- Fasting blood sugar test: A blood sample will be taken after an overnight fast. A fasting blood sugar level less than 100 mg/dL (5.6 mmol/L) is normal. A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. If it”s 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes mellitus. From 100 mg/dL (5.6 mmol/L) to 125 mg/dL (6.9 mmol/L) is considered prediabetes, which puts you at greater risk of developing diabetes.
- Oral glucose tolerance test: For this test, you fast overnight, and the fasting blood sugar level is measured. Then you drink a sugary liquid, and blood sugar levels are tested periodically for the next several hours. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal. A reading of more than 200 mg/dL (11.1 mmol/L) after two hours indicates diabetes. A reading between 140 and 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) indicates prediabetes.
Treatments and drugs
Treatment for diabetes mellitus type 2 requires a lifelong commitment to:
- Blood sugar monitoring
- Healthy eating
- Regular exercise
- Possibly, diabetes medication or insulin therapy
These steps will help keep your blood sugar level closer to normal, which can delay or prevent complications.
- Monitoring your blood sugar: Depending on your treatment plan, you may check and record your blood sugar level once a day or several times a week. Ask your doctor how often he or she wants you to check your blood sugar. Careful monitoring is the only way to make sure that your blood sugar level remains within your target range.
- Healthy eating: Contrary to popular perception, there”s no diabetes diet. You won”t be restricted to a lifetime of boring, bland foods. Instead, you”ll need plenty of:
– Fruits
– Vegetables
– Whole grains
These foods are high in nutrition and low in fat and calories. You”ll also need to eat fewer animal products and sweets.
Counting carbohydrates in your food is another thing you”ll need to incorporate into meal planning.
Low glycemic index foods also may be helpful. The glycemic index is a measure of how quickly a food causes a rise in your blood sugar.
- Physical activity: Everyone needs regular aerobic exercise, and people who have diabetes mellitus type 2 are no exception. Get your doctor”s OK before you start an exercise program. Then choose activities you enjoy, such as walking, swimming or biking. What”s most important is making physical activity part of your daily routine. Aim for at least 30 minutes of aerobic exercise most days of the week. Stretching and strength training exercises are important, too. If you haven”t been active for a while, start slowly and build up gradually.
- Diabetes medications and insulin therapy: Some people who have diabetes mellitus type 2 can manage their blood sugar with diet and exercise alone, but many need diabetes medications or insulin therapy. Some studies indicate that early intervention with medication, even before the A1C is significantly elevated, may improve control of blood sugar levels over time. The decision about which medications are best depends on many factors, including your blood sugar level and the presence of any other health problems. Your doctor might even combine drugs from different classes to help you control your blood sugar in several different ways.
