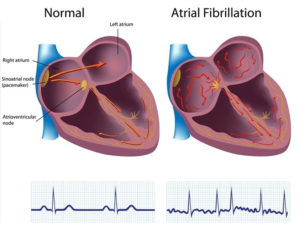
 Atrial fibrillation is the most common irregular heart rhythm that starts in the atria. Instead of the SA node (sinus node) directing the electrical rhythm, many different impulses rapidly fire at once, causing a very fast, chaotic rhythm in the atria. Because the electrical impulses are so fast and chaotic, the atria cannot contract and/or squeeze blood effectively into the ventricle.
Atrial fibrillation is the most common irregular heart rhythm that starts in the atria. Instead of the SA node (sinus node) directing the electrical rhythm, many different impulses rapidly fire at once, causing a very fast, chaotic rhythm in the atria. Because the electrical impulses are so fast and chaotic, the atria cannot contract and/or squeeze blood effectively into the ventricle.
Instead of the impulse traveling in an orderly fashion through the heart, many impulses begin at the same time and spread through the atria, competing for a chance to travel through the AV node. The AV node limits the number of impulses that travel to the ventricles, but many impulses get through in a fast and disorganized manner. The ventricles contract irregularly, leading to a rapid and irregular heartbeat. The rate of impulses in the atria can range from 300 to 600 beats per minute.
What causes atrial fibrillation?
There is no one “cause” of atrial fibrillation, although it is associated with many conditions, including:
Most common causes
- Hypertension
- Coronary artery disease
- Heart valve disease
- After heart surgery
- Chronic lung disease
- Heart failure
- Cardiomyopathy
- Congenital heart disease
- Pulmonary embolism
Less common causes
- Hyperthyroidism
- Pericarditis
- Viral infection
In at least 10 percent of the cases, no underlying heart disease is found. In these cases, AF may be related to alcohol or excessive caffeine use, stress, certain drugs, electrolyte or metabolic imbalances, severe infections, or genetic factors. In some cases, no cause can be found.
The risk of AF increases with age, particularly after age 60.
How is atrial fibrillation diagnosed?
The most commonly used tests to diagnose atrial fibrillation include:
Electrocardiogram: The ECG draws a picture on graph paper of the electrical impulses traveling through the heart muscle. An EKG provides an electrical “snapshot” of the heart.
Holter monitor: A small external recorder is worn over a short period of time, usually one to three days. Electrodes are placed on the skin of your chest. Wires are attached from the electrodes to the monitor. The electrical impulses are continuously recorded and stored in the monitor. After the monitor is removed, a technician uses a computer to analyze the data to evaluate the heart’s rhythm.
Portable event monitor: A monitor that is worn for about a month for patients who have less frequent irregular heartbeat episodes and symptoms. Electrodes are placed on the skin of your chest. Wires are attached from the electrodes to the monitor. The patient presses a button to activate the monitor when symptoms occur. The device records the electrical activity of the heart for several seconds. The patient then transmits the device’s recorded information over a telephone line to the doctor’s office for evaluation. The portable event monitor is very useful in determining what heart rhythm is causing your symptoms.
Transtelephonic monitor: When you develop symptoms of atrial fibrillation, a strip of your current heart rhythm can be transmitted to your doctor’s office over the telephone, using a monitor with two bracelets or by placing the monitor against your chest wall.
What are the dangers of atrial fibrillation?
Some people live for years with atrial fibrillation without problems. However, atrial fibrillation can lead to future problems:
- Because the atria are beating rapidly and irregularly, blood does not flow through them as quickly. This makes the blood more likely to clot. If a clot is pumped out of the heart, it can travel to the brain, resulting in a stroke. People with atrial fibrillation are 5 to 7 times more likely to have a stroke than the general population. Clots can also travel to other parts of the body (kidneys, heart, intestines), and cause other damage.
- Atrial fibrillation can decrease the heart’s pumping ability. The irregularity can make the heart work less efficiently. In addition, atrial fibrillation that occurs over a long period of time can significantly weaken the heart and lead to heart failure.
- Atrial fibrillation is associated with an increased risk of stroke, heart failure and even death.
What are the symptoms of atrial fibrillation?
You may have atrial fibrillation without having any symptoms. If you have symptoms, they may include:
Heart palpitations – Sudden pounding, fluttering or racing sensation in the chest
Lack of energy or feeling over-tired
Dizziness – Feeling light-headed or faint
Chest discomfort – Pain, pressure or discomfort in the chest
Shortness of breath – Having difficulty breathing during normal activities and even at rest
How is atrial fibrillation treated?
The goals of treatment for atrial fibrillation include regaining a normal heart rhythm, controlling the heart rate, preventing blood clots and reducing the risk of stroke.
Many options are available to treat atrial fibrillation, including lifestyle changes, medications, catheter-based procedures and surgery. The type of treatment that is recommended for you is based on your heart rhythm and symptoms.
Lifestyle Changes
In addition to taking medications, there are some changes you can make to improve your heart health.
- If your irregular heart rhythm occurs more often with certain activities, tell your doctor. Sometimes, your medications may need to be adjusted.
- Quit smoking.
- Limit your intake of alcohol. Moderation is the key. Ask your doctor for specific alcohol guidelines.
- Limit the use of caffeine. Some people are sensitive to caffeine and may notice more symptoms when using caffeinated products (such as tea, coffee, colas and some over-the-counter medications).
- Beware of stimulants used in cough and cold medications, as some of these medications contain ingredients that may increase the risk of irregular heart rhythms.
Procedures for Atrial Fibrillation
When drugs do not work to correct or control atrial fibrillation, or when medications are not tolerated, a procedure may be necessary, such as: electrical cardioversion, pulmonary vein isolation, catheter ablation of the AV node, or device therapy.
What Is Electrical Cardioversion?
Electrical cardioversion frequently restores a normal rhythm, although its effect may not be permanent. After a short-acting anesthesia is given, a machine is used to deliver an electric shock through electrode patches placed on the chest to synchronize the heartbeat and restore a normal rhythm. Although this procedure only takes a few seconds, several attempts may be needed to restore a normal rhythm. A patient may need to be on Coumadin for at least three weeks before this procedure is performed. This decreases the risk of a stroke that can occur with the cardioversion.
What Is Catheter Ablation Therapy?
Catheter ablation therapy is an option for people who cannot tolerate medications or when drugs fail to maintain the normal heart rhythm.
Pulmonary vein isolation:
During this procedure, special catheters are inserted into the heart. Research has shown that most atrial fibrillation signals come from the four pulmonary veins as they enter the left atrium.
A specialized viewing device called intracardiac echocardiography is used to visualize the left atrium during the procedure. One catheter in the left atrium is used to map or locate the abnormal impulses coming from the pulmonary veins. The other catheter is used to deliver the radiofrequency energy to create lesions outside the pulmonary veins. The procedure is repeated for all four pulmonary veins.
The lesions heal within four to eight weeks and form a circular scar around the pulmonary veins. The scar blocks any impulses firing from within the pulmonary veins, thereby “disconnecting” the pathway of the abnormal rhythm and curing atrial fibrillation.
Ablation of the AV node:
During this procedure, the doctor applies radiofrequency energy to injure the AV node. The end result is a permanent, very slow heart rate, since the electrical impulses from the top chamber of the heart cannot travel down to the lower chamber. Therefore, the patient needs a permanent pacemaker to maintain an adequate heart rate.
What Is a Permanent Pacemaker?
A pacemaker is a device that sends electrical impulses to the heart muscle to maintain a specified heart rate. Pacemakers may be implanted in people with AF who have a slow heart rate. The pacemaker has a pulse generator and leads (wires) that send impulses from the pulse generator to the heart muscle, as well as sense the heart”s electrical activity.
What Is Surgical Therapy?
Patients with chronic atrial fibrillation not relieved by medication or procedures, or patients who have other conditions requiring heart surgery, may be candidates for surgical treatment of AF. These procedures are types of open-heart surgery that require general anesthesia and a hospital stay.
During the Maze procedure, a series of precise incisions are made in the right and left atria to confine the electrical impulses to defined pathways to reach the AV node.
Surgical pulmonary vein isolation is a modification of the Maze procedure in which the surgeon uses alternative energy sources instead of incisions to create lesions. The alternative energy sources used during surgical pulmonary vein isolation include: radiofrequency, cryothermy, microwave, and laser. The goal of all four energy sources is to produce lesions and ultimately scar tissue to block the abnormal electrical impulses from being conducted through the heart and to promote the normal conduction of impulses through the proper pathway.
Many of these approaches can be performed with minimally invasive (endoscopic or “keyhole”) surgical techniques.
Radiofrequency Ablation:
A special radiofrequency energy catheter is used to heat the tissue and produce lesions on the heart similar to the lesions of the Maze procedure. There are a variety of surgical techniques related to the type of catheter used, the dose of energy, and the types of lesions created.
Cryothermy:
Very cold temperatures are transmitted through a probe (called a cryoprobe) to create lesions. This technique is used commonly during arrhythmia surgery to replace the incisions made during the Cox Maze procedure.
Microwave Technology:
A special wand-like catheter is used to direct microwave energy to create several lesions on the heart. The lesions block the conduction of abnormal electrical beats and restore a normal heartbeat.
Laser:
Lasers rapidly create the lesions or lines of conduction block. Laser technology offers promise for the development of additional minimally invasive approaches.
Some patients may have atrial fibrillation in addition to other heart problems (such as valve or coronary artery disease) which require surgery. In these cases, the surgeon may combine the surgeries to correct the atrial fibrillation and the coexisting heart condition at the same time.
