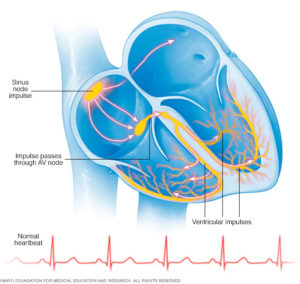
 Arrhythmias are heart rhythm problems that occur when the electrical impulses in your heart that coordinate your heartbeats don”t work properly, causing your heart to beat too fast, too slow or irregularly.
Arrhythmias are heart rhythm problems that occur when the electrical impulses in your heart that coordinate your heartbeats don”t work properly, causing your heart to beat too fast, too slow or irregularly.
Heart arrhythmias are often harmless. Most people have occasional, irregular heartbeats that may feel like a fluttering or racing heart. However, some heart arrhythmias may cause bothersome signs and symptoms.
Symptoms
Arrhythmias may not cause any signs or symptoms. In fact, Dr Villa might find you have an arrhythmia before you do, during a routine examination.
Some people do have noticeable arrhythmia symptoms, which may include:
- A fluttering in your chest
- A racing heartbeat (tachycardia)
- A slow heartbeat (bradycardia)
- Chest pain
- Shortness of breath
- Lightheadedness
- Dizziness
- Fainting (syncope) or near fainting
What Causes an Arrhythmia?
Arrhythmias may be caused by many different factors, including:
- Coronary artery disease.
- Electrolyte imbalances in your blood (such as sodium or potassium).
- Changes in your heart muscle.
- Injury from a heart attack.
- Healing process after heart surgery.
- Irregular heart rhythms can also occur in otherwise normal, healthy hearts.
What Are the Types of Arrhythmias?
The types of arrhythmias include:
Premature atrial contractions: These are early extra beats that originate in the atria (upper chambers of the heart). They are harmless and generally do not require treatment.
Premature Ventricular Contractions(PVCs): These are among the most common arrhythmias and occur in people with or without heart disease. This is the skipped heartbeat we all occasionally experience. In some people, it can be related to stress, too much caffeine or nicotine, or too much exercise. But sometimes, PVCs can be caused by heart disease or electrolyte imbalance. People who have a lot of PVCs, and/or symptoms associated with them, should be evaluated by a heart doctor. However, in most people, PVCs are usually harmless and rarely need treatment.
Atrial Fibrillation: Is a very common irregular heart rhythm that causes the atria, the upper chambers of the heart, to contract abnormally.
Atrial Flutter: This is an arrhythmia caused by one or more rapid circuits in the atrium. Atrial flutter is usually more organized and regular than atrial fibrillation. This arrhythmia occurs most often in people with heart disease and in the first week after heart surgery. It often converts to atrial fibrillation.
Paroxysmal Supraventricular Tachycardia (PSVT): A rapid heart rate, usually with a regular rhythm, originating from above the ventricles. PSVT begins and ends suddenly. There are two main types: accessory path tachycardias and AV nodal reentrant tachycardias.
Accessory Pathway Tachycardias: A rapid heart rate due to an extra abnormal pathway or connection between the atria and the ventricles. The impulses travel through the extra pathways as well as through the usual route. This allows the impulses to travel around the heart very quickly, causing the heart to beat unusually fast.
AV Nodal Reentrant Tachycardia: A rapid heart rate due to more than one pathway through the AV node. It can cause heart palpitations, fainting, or heart failure. In some cases, it can be terminated using simple maneuvers, such as breathing in and bearing down. Some drugs can also stop this heart rhythm.
Ventricular Tachycardia (V-tach): A rapid heart rhythm originating from the lower chambers (or ventricles) of the heart. The rapid rate prevents the heart from filling adequately with blood. This can be a serious arrhythmia, especially in people with heart disease, and may be associated with more symptoms.
Ventricular Fibrillation: An erratic, disorganized firing of impulses from the ventricles. The ventricles quiver and are unable to contract or pump blood to the body. This is a medical emergency that must be treated with cardiopulmonary resuscitation (CPR) and defibrillation as soon as possible.
Long QT Syndrome: The QT interval is the area on the electrocardiogram that represents the time it takes for the heart muscle to contract and then recover, or for the electrical impulse to fire impulses and then recharge. When the QT interval is longer than normal, it increases the risk of a life-threatening form of ventricular tachycardia. Long QT syndrome is an inherited condition that can cause sudden death in young people. It can be treated with antiarrhythmic drugs, pacemaker, electrical cardioversion, defibrillation, implanted cardioverter/defibrillator, or ablation therapy.
Bradyarrhythmias: These are slow heart rhythms, which may arise from disease in the heart”s electrical conduction system. Examples include sinus node dysfunction and heart block.
Sinus node Dysfunction: A slow heart rhythm due to an abnormal sinus node. Significant sinus node dysfunction that causes symptoms is treated with a pacemaker.
Heart Block: A delay or complete block of the electrical impulse as it travels from the sinus node to the ventricles. The heart may beat irregularly and, often, more slowly. If serious, heart block is treated with a pacemaker.
Risk factors
Certain factors may increase your risk of developing an arrhythmia. These include:
- Coronary artery disease
- High blood pressure
- Congenital heart disease
- Thyroid problems
- Drugs and supplements
- Obesity
- Diabetes
- Obstructive sleep apnea
- Electrolyte imbalance
- Drinking too much alcohol
- Caffeine or nicotine use
Complications
Certain arrhythmias may increase your risk of developing conditions such as:
Stroke. When your heart quivers, it”s unable to pump blood effectively, which can cause blood to pool. This can cause blood clots to form. If a clot breaks loose, it can travel to and obstruct a brain artery, causing a stroke. This may damage a portion of your brain or lead to death. For people who have atrial fibrillation, the medications warfarin (Coumadin) or dabigatran (Pradaxa) may help prevent blood clots, which can cause a stroke.
Heart failure. This can result if your heart is pumping ineffectively for a prolonged period due to a bradycardia or tachycardia, such as atrial fibrillation. Sometimes, controlling the rate of an arrhythmia that”s causing heart failure can improve your heart”s function.
Tests and Diagnosis
To diagnose a heart arrhythmia, Dr. Villa may ask about or test for conditions that may trigger your arrhythmia, such as heart disease or a problem with your thyroid gland. Dr. Villa may also perform heart-monitoring tests specific to arrhythmias. These may include:
Electrocardiogram (ECG). During an ECG, sensors (electrodes) that can detect the electrical activity of your heart are attached to your chest and sometimes to your limbs. An ECG measures the timing and duration of each electrical phase in your heartbeat.
Holter monitor. This portable ECG device can be worn for a day or more to record your heart”s activity as you go about your routine.
Event monitor. For sporadic arrhythmias, you keep this portable ECG device at home, attaching it to your body and using it only when you have symptoms of an arrhythmia. This lets your doctor check your heart rhythm at the time of your symptoms.
Echocardiogram. In this noninvasive test, a hand-held device (transducer) placed on your chest uses sound waves to produce images of your heart”s size, structure and motion.
Cardiac Computerized Tomography (CT) or Magnetic Resonance Imaging (MRI). These tests can be used to diagnose heart problems that might cause heart arrhythmias. In a cardiac CT scan, you lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest.
If Dr. Villa do not find an arrhythmia during those tests, he may try to trigger your arrhythmia with other tests, which may include:
- Stress test.
- Tilt table test.
- Electrophysiological testing and mapping.
Treatment
Most arrhythmias are considered harmless and are left untreated. Once Dr. Villa has documented that you have an arrhythmia, he will need to find out whether it”s abnormal or merely reflects the heart”s normal processes. He will also determine whether your arrhythmia is clinically significant that is, whether it causes symptoms or puts you at risk for more serious arrhythmias or complications of arrhythmias in the future. If your arrhythmia is abnormal and clinically significant, Dr. Villa will set a treatment plan.
Treatment goals:
- Prevent blood clots from forming to reduce stroke risk.
- Control your heart rate within a relatively normal range.
- Restore a normal heart rhythm, if possible.
- Treat heart disease/condition that may be causing arrhythmia.
- Reduce other risk factors for heart disease and stroke.
Lifestyle and home remedies
Many arrhythmias can be blamed on underlying heart disease, so Dr. Villa may suggest that, in addition to other treatments, you make lifestyle changes that will keep your heart as healthy as possible. Making healthy lifestyle changes can also help prevent heart arrhythmias from developing in the first place.
These lifestyle changes may include:
- Eat heart-healthy foods.
- Increase your physical activity.
- Quit smoking.
- Cut back on caffeine and alcohol.
- Find ways to reduce the amount of stress in your life.
- Avoid stimulant medications, such as medications found in over-the-counter treatments for colds and nasal congestion.
