What is superficial venous reflux?
Superficial venous reflux is a condition that develops when the valves that usually keep blood flowing out of your legs become damaged or diseased. This causes blood to pool in your legs. Common symptoms of superficial venous reflux include pain, swelling, leg heaviness and fatigue, as well as varicose veins in your legs.
What are Varicose Veins?
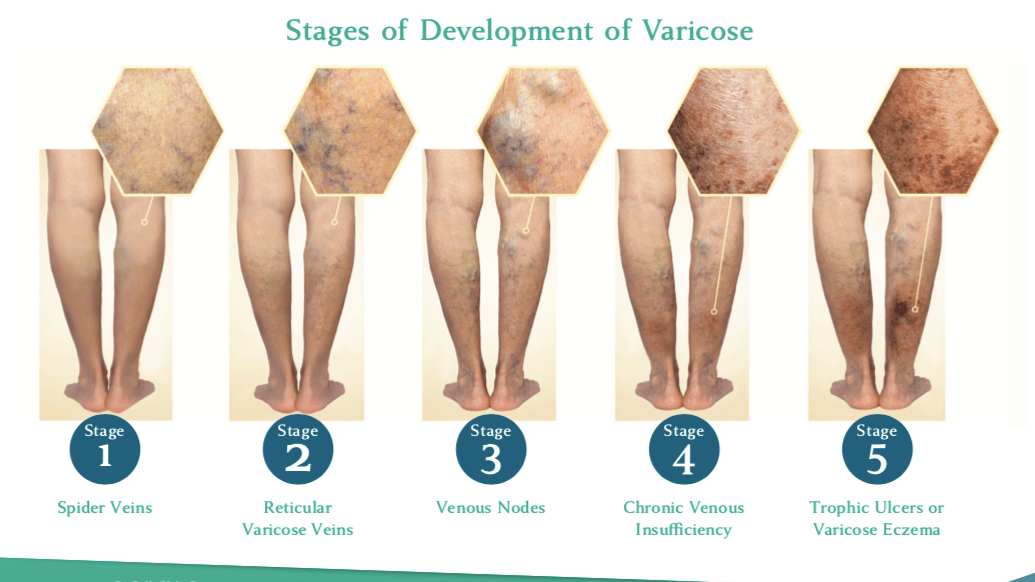
Varicose veins are most often swollen, gnarled veins that most frequently occur in the legs, ankles and feet. They are produced by a condition known as venous insufficiency or venous reflux, in which blood circulating through the lower limbs does not properly return to the heart but instead pools up in the distended veins.
More than 25 million Americans suffer from venous reflux disease. The symptoms can include pain and fatigue in the legs, swollen ankles and calves, burning or itching skin, skin discoloration and leg ulcers. In less severe cases, thin, discolored vessels – “spider veins” – may be the only symptom.
Gender and age are two primary risk factors in the development of venous reflux. An estimated 72% of American women and 42% of men will experience varicose veins symptoms by the time they reach their sixties. Women who have been pregnant more than once and people who are obese, have a family history of varicose veins or spend a great deal of time standing have an elevated risk for the condition, but it can occur in almost anyone at almost any age. Varicose veins never go away without treatment and frequently progress and worsen over time.
Severe varicose veins can have a significant impact on the lives of people who work on their feet – nurses, teachers, flight attendants et al. Research has shown that more than two million workdays are lost each year in the US, and annual expenditures for treatment total $1.4 billion.
What are Spider Veins?
Spider veins, also known medically as telangiectasia or venulectasias, are the mildest manifestation of venous insufficiency, similar to varicose veins but smaller. They are small, often tangled groups of tiny blood vessels just under the skin surface that frequently resemble spider webs or tree branches. They are generally red, blue or purple and are clearly visible, usually on the thighs, lower legs and face. Spider veins can sometimes cover large areas of skin, but they are a cosmetic problem only, rarely causing physical symptoms. At least a third of all women and a smaller percentage of men are believed to display the condition.
Spider veins are capillaries, thin vessels directly connected with the larger venous system, and like varicose veins they are caused by venous reflux. Spider veins may be isolated or associated with “feeder” veins or with larger underlying varicose veins, but they are not varicose veins – they do not bulge above the skin surface and do not require medical treatment.
Spider veins can be diagnosed merely by sight. They tend to take on one of three characteristic patterns – a “sunburst” or spider-web pattern radiating outward from a central point, a “tree-branch” pattern, or a “matting” or linear pattern that may be nothing more than a set of thin lines. Even in the absence of physical discomfort, some physicians observing spider veins prefer to conduct ultrasound exams to determine the extent of the problem and the underlying causes of the condition.
Risk factors for spider veins are similar to those for varicose veins – age, heredity, pregnancy, hormonal changes, obesity and extended periods of standing – as well as sun exposure, particularly in fair-skinned people, and injuries to the skin surface. Some physicians believe that exercise, weight loss and the wearing of support hose and flat shoes instead of high heels can reduce the incidence of spider veins.
Spider vein treatments are non-invasive or minimally invasive and include sclerotherapy and laser procedures. They are considered cosmetic procedures and are not covered by health insurance or Medicare unless a more serious underlying condition is diagnosed
What is the Difference Between Varicose Veins and Spider Veins?
Varicose veins and spider veins are both visible surface symptoms of venous insufficiency, the inability of diseased leg veins to push blood back up towards the heart. The surface veins become distended and prominent because blood that should normally circulate through the body is instead accumulating in the legs.
Varicose Veins
Varicose veins are a medical condition, larger and more serious manifestations of venous reflux disease. The swollen vessels can protrude several millimeters beyond the skin surface and can become knotted and tangled. Varicose veins are frequently accompanied by clinical symptoms such as pain, throbbing, burning sensations, muscle cramps and fatigue, and can progress to leg ulcers, blood clots and other health-endangering conditions.
Spider Veins
Spider veins are thin surface veins that turn blue or red under the strain of the venous reflux and affect the appearance of the location where they occur. Spider veins are considered a cosmetic problem, rarely causing physical discomfort, and can be addressed with a variety of non-invasive, techniques.
What is the difference between cosmetic surgery and medical necessity?
Physicians have been debating the treatment of varicose veins for well over two thousand years – the legendary Hippocrates himself wrote about them in the fifth century BC – but today both medical necessity and health insurance are major factors in determining the course of treatment for the condition.
When varicose or spider veins are treated for the exclusive purpose of improving the patient’s appearance, it is considered cosmetic surgery and will not be covered by the patient’s health insurance or Medicare. Virtually all procedures addressing spider veins will fall into this category.
If, however, the varicose veins are causing symptoms like pain, swelling, fatigue or other symptoms that affect the patient’s ability to work or function normally, or if the underlying venous reflux disease is producing complications like skin ulcers or blood clots, a physician can determine that treatment is required to restore or preserve the patient’s health and well-being, and is therefore considered a medical necessity. Under those circumstances, most health insurance and Medicare plans will cover the procedure.
