What is Percutaneous Transluminal Coronary Angioplasty (PTCA)?
For certain people, heart disease treatment can be achieved without surgery. Percutaneous Transluminal Coronary Angioplasty or Ballon Angioplasty is a non-surgical procedure that can be used to open blocked heart arteries. Stent placement is another option that can be done during a Percutaneous Transluminal Coronary Angioplasty.
The procedure is performed in the cardiac catheterization laboratory (or cath lab) by Dr. Augusto Villa and a team of cardiovascular nurses and technicians.
First, a cardiac catheterization is performed before an Angioplasty.
What is a cardiac catheterization?
Cardiac catheterization, also called cardiac cath or coronary angiogram, is an invasive imaging procedure that allows Dr. Villa to evaluate your heart function.
Cardiac catheterization is used to:
- Evaluate or confirm the presence of coronary artery disease, valve disease or disease of the aorta.
- Evaluate heart muscle function.
- Determine the need for further treatment (such as an interventional procedure or coronary artery bypass graft, or CABG, surgery).
During a cardiac catheterization, a long, narrow tube called a catheter is inserted through a plastic introducer sheath (a short, hollow tube that is inserted into a blood vessel in your wrist or leg). The catheter is guided through the blood vessel to the coronary arteries with the aid of a special x-ray machine.
Contrast material is injected through the catheter and x-ray movies are created as the contrast material moves through the heart’s chambers, valves and major vessels. This part of the procedure is called a coronary angiogram (or coronary angiography). The digital photographs of the contrast material are used to identify the site of the narrowing or blockage in the coronary artery. Once the catheter engages the artery with the blockage, the doctor will perform an interventional procedure.
Additional imaging procedures, called intra-vascular ultrasound (IVUS) and fractional flow reserve (FFR), may be performed along with cardiac catheterization in some cases to obtain detailed images of the walls of the blood vessels. Both of these imaging procedures are currently only available in specialized hospitals and research centers.
With IVUS, a miniature sound-probe (transducer) is positioned on the tip of a coronary catheter. The catheter is threaded through the coronary arteries and, using high-frequency sound waves, produces detailed images of the inside walls of the arteries. IVUS produces an accurate picture of the location and extent of plaque.
What is an interventional cardiology procedure?
An interventional cardiology procedure is a non-surgical treatment used to open narrowed coronary arteries to improve blood flow to the heart. An interventional cardiology procedure can be performed during a diagnostic cardiac catheterization when a blockage is identified, or it may be scheduled after a catheterization has confirmed the presence of coronary artery disease.
An interventional cardiology procedure starts out the same way as a cardiac catheterization. Once the catheter is in place, one of these interventional procedures is performed to open the artery:
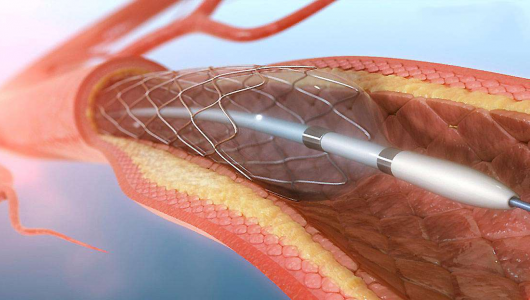
- Percutaneous Transluminal Coronary Angioplasty (PTCA) or Balloon Angioplasty: A procedure in which a small balloon at the tip of the catheter is inserted near the blocked or narrowed area of the coronary artery. When the balloon is inflated, the fatty plaque or blockage is compressed against the artery walls and the diameter of the blood vessel is widened (dilated) to increase blood flow to the heart. This procedure is sometimes complicated by vessel recoil and restenosis.
- Percutaneous Transluminal Coronary Angioplasty with stenting: In most cases, balloon angioplasty is performed in combination with the stenting procedure. A stent is a small metal mesh tube that acts as a scaffold to provide support inside your coronary artery. A balloon catheter, placed over a guide wire, is used to insert the stent into the narrowed coronary artery. Once in place, the balloon tip is inflated and the stent expands to the size of the artery and holds it open. The balloon is then deflated and removed while the stent stays in place permanently. Over a several-week period, your artery heals around the stent. Stents are commonly placed during interventional procedures such as angioplasty to help keep the coronary artery open. Some stents contain medicine and are designed to reduce the risk of reblockage (restenosis). Dr Villa will determine if this type of stent is appropriate for your type of blockage.
- Rotablation: A special catheter, with an acorn-shaped, diamond-coated tip, is guided to the point of narrowing in your coronary artery. The tip spins around at a high speed and grinds away the plaque on your artery walls. The microscopic particles are washed safely away in your blood stream and filtered out by your liver and spleen. This process is repeated as needed to allow for better blood flow. This procedure is rarely used today because balloon angioplasty and stenting have much better results and are technically easier for the cardiologist to perform.
- Cutting Balloon: The cutting balloon catheter has a special balloon tip with small blades. When the balloon is inflated, the blades are activated. The small blades score the plaque, then the balloon compresses the fatty matter into the artery wall.
What Can I Expect Before a Percutaneous Transluminal Coronary Angioplasty?
Before an angioplasty, most people will need to have a routine chest X-ray, blood test, electrocardiogram and urinalysis. These tests may require separate appointments and are usually scheduled the day before the procedure.
You will not be able to eat or drink after midnight the evening before the procedure.
If you normally wear dentures or a hearing assistive device, plan to wear them during your angioplasty to help with communication. If you wear glasses, bring them also.
Please tell Dr. Villa if you are taking Coumadin (warfarin), diuretics (water pills), or insulin. Also let him know if you are allergic to anything, especially iodine, shellfish, X-ray dye, latex or rubber products (such as rubber gloves or balloons), or penicillin-type medications.
You will need to take aspirin before the procedure. Please tell Dr. Villa if you did not take aspirin. You will remain awake during an angioplasty, but you are given medication to help you relax.
What Happens After a Percutaneous Transluminal Coronary Angioplasty?
After your angioplasty, you will have to lay flat (without bending your legs) while the groin sheath is in place. A sheet may be placed across your leg with the sheath to remind you to keep it straight.
After the groin sheath is removed, you must lay flat for about six hours to prevent bleeding, but your nurse can raise your head (about two pillows high) after two hours. The nurse will tell you when you can get out of bed with assistance six to eight hours after the groin sheath is removed (or sooner if a collagen “plug” was placed in your artery).
You should not eat or drink anything except clear liquids until the groin sheath is removed because nausea can occur during this time. Once you are allowed to eat, you will be advised to follow a low-cholesterol and low-salt diet. You may be admitted to the hospital overnight for observation after the procedure.
Notify Dr. Villa immediately if you develop a fever or experience chest pain, swelling, or pain in your groin or leg. If you experience bleeding from your groin site after you return home, call 9-1-1 and lie down immediately. Remove the dressing and push down on your pulse in the affected area.
When you have recovered sufficiently from the procedure and have talked with Dr. Villa about your follow-up care, you will be able to go home.
You will need to take it easy for a few days after an angioplasty. You may climb stairs, but use a slower pace. Do not strain during bowel movements.
Gradually increase your activities until you reach your normal activity level by the end of the week.
Who performs the procedures?
Dr. Villa, a cardiovascular invasive physician, has all the training, qualifications and required board certifications to perform a successful cardiac catheterization and interventional procedures.
How long do the procedures take to perform?
The cardiac catheterization procedure itself generally takes 30 minutes, but the preparation and recovery time add several hours to your appointment time (5 to 9 hours or longer).
An interventional procedure usually takes from 90 to 120 minutes, but the preparation and recovery time add several hours. If you had previous coronary artery bypass graft (CABG) surgery, you can expect your interventional procedure to last longer. Plan on staying at the Hospital all day for the procedure and remaining in the hospital overnight.
What are the possible risks of the procedures?
If you need to have a cardiac catheterization or an interventional procedure, Dr. Villa will discuss the specific risks and potential benefits of the recommended procedure with you.
Some of the possible risks of cardiac catheterization and interventional procedures include:
- Allergic reaction to the medication or contrast material used during the procedure Irregular.
- Irregular heart rhythm.
- Infection.
- Bleeding at the catheter insertion site.
- Continued chest pain or angina.
- Mild to moderate skin reactions (like sun-burn) from X-ray exposure.
- Kidney Failure.
- Heart attack, blood clots, stroke or death.
- Acute closure of coronary artery.
- Emergency coronary artery bypass graft (CABG) surgery.
There may be other possible risks. When you meet with Dr. Villa, please ask questions to make sure you understand why the procedure is recommended and what all of the potential risks are.
Does an interventional procedure cure coronary artery disease?
For most people, interventional procedures increase blood flow to the heart, diminish chest pain and decrease the risk of a heart attack.
Although an interventional procedure opens up blocked arteries, it does not CURE coronary artery disease. You will still need to reduce your risk factors and make certain lifestyle changes to prevent future disease development or progression.
To achieve the best results, you must be committed to leading a heart-healthy lifestyle. Your health care team can help you achieve your goals, but it is up to you to take your medications as prescribed, make dietary changes, quit smoking, exercise regularly, keep your follow-up appointments and be an active member of the treatment team.
